About 1.2% of people will be diagnosed with thyroid cancer during their lifetime. In the past 40 years, due to the widespread use of imaging and the introduction of fine needle puncture biopsy, the detection rate of thyroid cancer has increased significantly, and the incidence of thyroid cancer has increased threefold. The treatment of thyroid cancer has progressed rapidly in the past 5 to 10 years, with a variety of new protocols gaining regulatory approval
Exposure to ionizing radiation during childhood was most strongly associated with papillary thyroid cancer (1.3 to 35.1 cases /10,000 person-years). A cohort study that screened 13,127 children under 18 years of age living in Ukraine after the 1986 Chernobyl nuclear accident for thyroid cancer found a total of 45 cases of thyroid cancer with an excess relative risk of 5.25/Gy for thyroid cancer. There is also a dose-response relationship between ionizing radiation and thyroid cancer. The younger the age at which ionizing radiation was received, the higher the risk of developing radiation-related thyroid cancer, and this risk persisted nearly 30 years after exposure.
Most risk factors for thyroid cancer are immutable: age, sex, race or ethnicity, and family history of thyroid cancer are the most important risk predictors. The older the age, the higher the incidence and the lower the survival rate. Thyroid cancer is three times more common in women than in men, a rate that is roughly constant worldwide. Genetic variation in the germ line of 25% of patients with medullary thyroid carcinoma is associated with inherited multiple endocrine tumor syndromes type 2A and 2B. 3% to 9% of patients with well-differentiated thyroid cancer have heritability.
Follow-up of more than 8 million residents in Denmark has shown that non-toxic nodular goiter is associated with an increased risk of thyroid cancer. In a retrospective cohort study of 843 patients undergoing thyroid surgery for unilateral or bilateral thyroid nodule, goiter, or autoimmune thyroid disease, higher preoperative serum thyrotropin (TSH) levels were associated with thyroid cancer: 16% of patients with TSH levels below 0.06 mIU/L developed thyroid cancer, while 52% of patients with TSH≥5 mIU/L developed thyroid cancer.
People with thyroid cancer often have no symptoms. A retrospective study of 1328 patients with thyroid cancer at 16 centers in 4 countries showed that only 30% (183/613) had symptoms at diagnosis. Patients with neck mass, dysphagia, foreign body sensation and hoarseness are usually more seriously ill.
Thyroid cancer traditionally presents as a palpable thyroid nodule. The incidence of thyroid cancer in palpable nodules is reported to be about 5% and 1%, respectively, in women and men in iodine-adequate areas of the world. At present, about 30% to 40% of thyroid cancers are found through palpation. Other common diagnostic approaches include non-thyroid related imaging (e.g., carotid ultrasound, neck, spine, and chest imaging); Patients with hyperthyroidism or hypothyroidism who have not touched the nodules receive thyroid ultrasonography; Patients with existing thyroid nodules were repeated with ultrasound; An unexpected discovery of occult thyroid cancer was made during post-operative pathologic examination.
Ultrasound is the preferred method of evaluation for palpable thyroid nodules or other imaging findings of thyroid nodules. Ultrasound is extremely sensitive in determining the number and characteristics of thyroid nodules as well as high-risk features associated with the risk of malignancy, such as marginal irregularities, punctate strong echoic focus, and extra-thyroid invasion.
At present, overdiagnosis and treatment of thyroid cancer is a problem that many doctors and patients pay special attention to, and clinicians should try to avoid overdiagnosis. But this balance is difficult to achieve because not all patients with advanced, metastatic thyroid cancer can feel thyroid nodules, and not all low-risk thyroid cancer diagnoses are avoidable. For example, an occasional thyroid microcarcinoma that may never cause symptoms or death can be diagnosed histologically after surgery for benign thyroid disease.
Minimally invasive interventional therapies such as ultrasound-guided radiofrequency ablation, microwave ablation and laser ablation offer a promising alternative to surgery when low-risk thyroid cancer requires treatment. Although the mechanisms of action of the three ablation methods are slightly different, they are basically similar in terms of tumor selection criteria, tumor response, and postoperative complications. Currently, most physicians agree that the ideal tumor feature for minimally invasive intervention is an internal thyroid papillary carcinoma < 10 mm in diameter and > 5 mm from heat-sensitive structures such as the trachea, esophagus, and recurrent laryngeal nerve. The most common complication after treatment remains inadvertent heat injury to the recurrent laryngeal nerve nearby, resulting in temporary hoarseness. To minimize damage to surrounding structures, it is recommended to leave a safe distance away from the target lesion.
A number of studies have shown that minimally invasive intervention in the treatment of thyroid papillary microcarcinoma has good efficacy and safety. Although minimally invasive interventions for low-risk papillary thyroid cancer have yielded promising results, most studies have been retrospective and focused on China, Italy, and South Korea. In addition, there was no direct comparison between the use of minimally invasive interventions and active surveillance. Therefore, ultrasound-guided thermal ablation is only suitable for patients with low-risk thyroid cancer who are not candidates for surgical treatment or who prefer this treatment option.
In the future, for patients with clinically significant thyroid cancer, minimally invasive interventional therapy may be another treatment option with a lower risk of complications than surgery. Since 2021, thermal ablation techniques have been used to treat patients with thyroid cancer below 38 mm (T1b~T2) with high-risk characteristics. However, these retrospective studies included a small cohort of patients (ranging from 12 to 172) and a short follow-up period (mean 19.8 to 25.0 months). Therefore, more research is needed to understand the value of thermal ablation in the treatment of patients with clinically important thyroid cancer.
Surgery remains the primary method of treatment for suspected or cytologically confirmed differentiated thyroid carcinoma. There has been controversy over the most appropriate scope of thyroidectomy (lobectomy and total thyroidectomy). Patients undergoing total thyroidectomy are at greater surgical risk than those undergoing lobectomy. Risks of thyroid surgery include recurrent laryngeal nerve damage, hypoparathyroidism, wound complications, and the need for thyroid hormone supplementation. In the past, total thyroidectomy was the preferred treatment for all differentiated thyroid cancers > 10 mm. However, a 2014 study by Adam et al. showed that there was no statistically significant difference in survival and recurrence risk between patients undergoing lobectomy and total thyroidectomy for 10 mm to 40 mm papillary thyroid cancer without clinically high-risk features.
Therefore, currently, lobectomy is usually preferred for unilateral well-differentiated thyroid cancer < 40 mm. Total thyroidectomy is generally recommended for well-differentiated thyroid cancer of 40 mm or larger and bilateral thyroid cancer. If the tumor has spread to regional lymph nodes, a dissection of the central and lateral lymph nodes of the neck should be performed. Only patients with medullary thyroid cancer and some well-differentiated large-volume thyroid cancers, as well as patients with external thyroid aggression, need prophylactic central lymph node dissection. Prophylactic lateral cervical lymph node dissection may be considered for patients with medullary thyroid cancer. In patients with suspected hereditary medullary thyroid carcinoma, plasma levels of norepinephrine, calcium, and parathyroid hormone (PTH) should be evaluated before surgery to identify MEN2A syndrome and avoid missing pheochromocytoma and hyperparathyroidism.
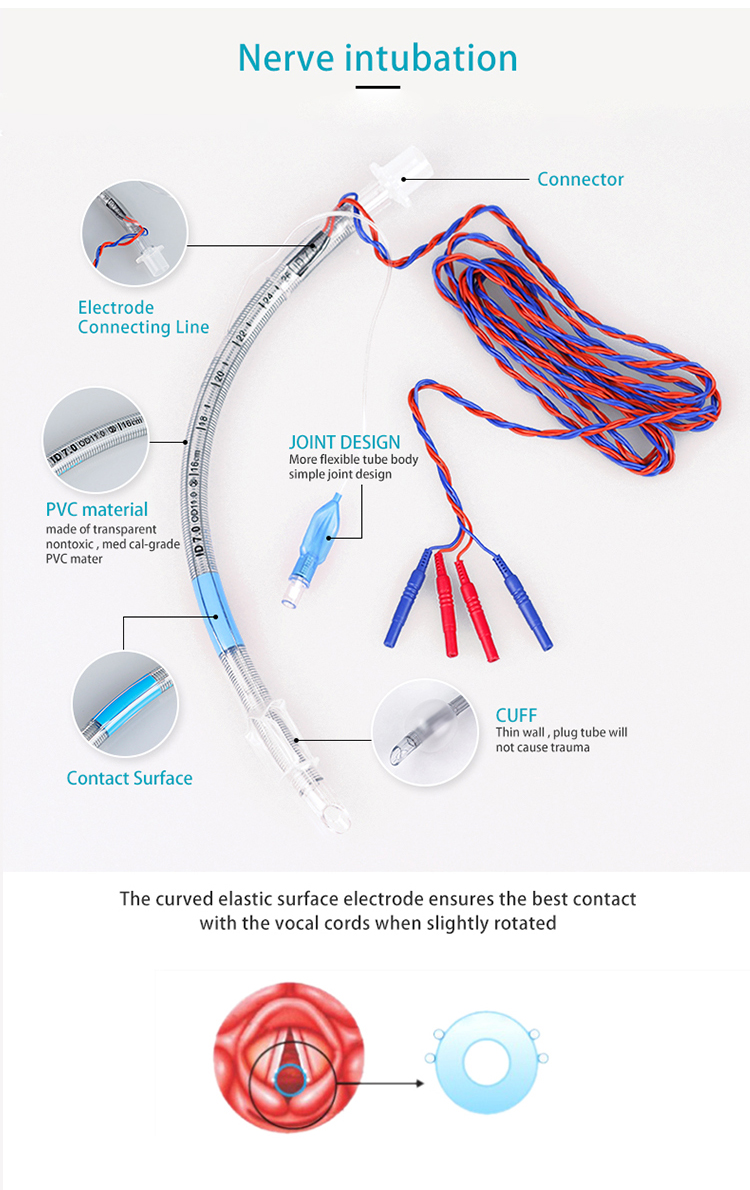
Nerve intubation is mainly used to connect with a suitable nerve monitor to provide an unobtrusive airway and to monitor intraoperative muscle and nerve activity in the larynx.
EMG Endotracheal Tube Product click here
Post time: Mar-16-2024