High blood pressure during pregnancy can lead to eclampsia and preterm birth and is a major cause of maternal and neonatal morbidity and death. As an important public health measure, the World Health Organization (WHO) recommends that pregnant women with inadequate dietary calcium supplements supplement 1000 to 1500 mg of calcium daily. However, due to the relatively cumbersome calcium supplement, the implementation of this recommendation is not satisfactory.
Randomized controlled trials conducted in India and Tanzania by Professor Wafie Fawzi of the Harvard School of Public Health in the United States found that low-dose calcium supplementation during pregnancy was no worse than high-dose calcium supplementation in reducing the risk of pre-eclampsia. In terms of reducing the risk of preterm birth, the Indian and Tanzanian trials had inconsistent results.
The two trials included 11,000 participants aged ≥18 years, gestational age < from November 2018 to February 2022 (India) and March 2019 to March 2022 (Tanzania). First-time mothers at 20 weeks who were expected to live in the trial area until 6 weeks postpartum were randomly assigned 1:1 to low-calcium supplementation (500 mg daily +2 placebo pills) or high-calcium supplementation (1500 mg daily) until delivery. The primary endpoints were preeclampsia and preterm birth (dual endpoints). Secondary endpoints included pregnancy-related hypertension, preeclampsia with severe manifestations, pregnancy-related death, stillbirth, stillbirth, low birth weight, small for gestational age, and neonatal death within 42 days. Safety endpoints included hospitalization of pregnant women (for reasons other than delivery) and severe anemia in the third trimester. Non-inferiority margins were relative risks of 1.54 (preeclampsia) and 1.16 (preterm birth), respectively.
For preeclampsia, the cumulative incidence of the 500 mg versus 1500 mg group in the Indian trial was 3.0% and 3.6%, respectively (RR, 0.84; 95% CI, 0.68~1.03); In the Tanzanian trial, the incidence was 3.0% and 2.7%, respectively (RR, 1.10; 95% CI, 0.88~1.36). Both trials showed that the risk of preeclampsia was not worse in the 500 mg group than in the 1500 mg group.
For preterm birth, in the Indian trial, the incidence of the 500 mg versus 1500 mg group was 11.4% and 12.8%, respectively (RR, 0.89; 95% CI, 0.80~0.98), the non-inferiority was established within the threshold value of 1.54; In the Tanzanian trial, preterm birth rates were 10.4% and 9.7%, respectively (RR, 1.07; 95% CI, 0.95~1.21), exceeded the non-inferiority threshold value of 1.16, and non-inferiority was not confirmed.
In both secondary and safety endpoints, there was no evidence that the 1500 mg group was better than the 500 mg group. A meta-analysis of the outcomes of the two trials found no differences between the 500 mg and 1500 mg groups in preeclampsia, preterm birth risk, and secondary and safety outcomes.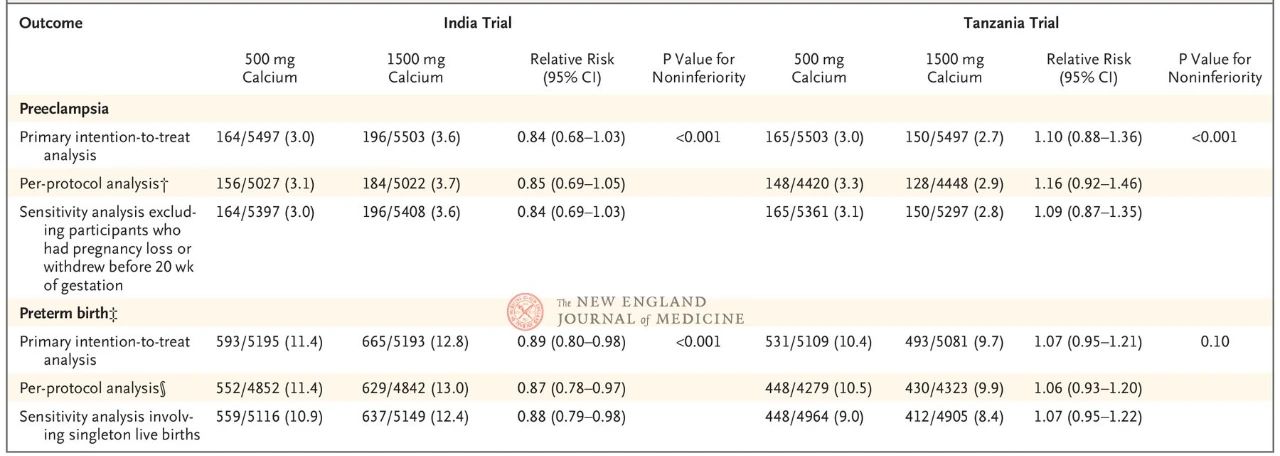
This study focused on the important public health issue of calcium supplementation in pregnant women for the prevention of preeclampsia, and conducted a large randomized controlled trial in two countries simultaneously to answer the important but still unclear scientific question of the optimal effective dose of calcium supplementation. The study had a rigorous design, large sample size, double-blind placebo, non-inferiority hypothesis, and two key clinical outcomes of preeclampsia and preterm birth as double endpoints, followed up to 42 days postpartum. At the same time, the quality of execution was high, the rate of loss of follow-up was very low (99.5% follow-up to pregnancy outcome, India, 97.7% Tanzania), and the compliance was extremely high: the median percentage of compliance was 97.7% (India, 93.2-99.2 interquartile interval), 92.3% (Tanzania, 82.7-97.1 interquartile interval).
Calcium is a necessary nutrient for fetal growth and development, and the demand for calcium in pregnant women increases compared with the general population, especially in the late pregnancy when the fetus grows rapidly and bone mineralization peaks, more calcium needs to be added. Calcium supplementation can also reduce the release of parathyroid hormone and intracellular calcium concentration in pregnant women, and reduce the contraction of blood vessels and uterine smooth muscle. Placebo-controlled trials have shown that high-dose calcium supplementation during pregnancy (> 1000 mg) reduced the risk of preeclampsia by more than 50% and the risk of preterm birth by 24%, and the reduction appeared to be even greater in people with low calcium intake. Therefore, in the “Recommended Recommendations for Calcium Supplementation during Pregnancy to Prevent Preeclampsia and its Complications” issued by the World Health Organization (WHO) in November 2018, it is recommended that people with low calcium intake should supplement calcium with 1500 to 2000 mg daily, divided into three oral doses, and several hours between taking iron to prevent preeclampsia. China’s Expert Consensus on Calcium Supplementation for Pregnant women, released in May 2021, recommends that pregnant women with low calcium intake supplement calcium 1000~1500 mg daily until delivery.
At present, only a few countries and regions have implemented the routine large-dose calcium supplement during pregnancy, the reasons include the large volume of calcium dosage form, difficult to swallow, complex administration plan (three times a day, and need to be separated from iron), and the medication compliance is reduced; In some areas, due to limited resources and high costs, calcium is not easy to obtain, so the feasibility of large dose calcium supplementation is affected. In clinical trials exploring low-dose calcium supplementation during pregnancy (mostly 500 mg daily), although compared with placebo, the risk of preeclampsia was reduced in the calcium supplementation group (RR, 0.38; 95% CI, 0.28~0.52), but it is necessary to be aware of the existence of research high risk bias [3]. In only one small clinical trial comparing low-dose and high-dose calcium supplementation, the risk of preeclampsia appeared to decrease in the high-dose group compared to the low-dose group (RR, 0.42; 95% CI, 0.18~0.96); There was no difference in the risk of preterm birth (RR, 0.31; 95% CI, 0.09~1.08)
Post time: Jan-13-2024




