The U.S. declaration of the end of the “public health emergency” is a milestone in the fight against SARS-CoV-2. At its peak, the virus killed millions of people around the world, completely disrupted lives and fundamentally changed healthcare. One of the most visible changes in the healthcare sector is the requirement for all personnel to wear masks, a measure aimed at implementing source control and exposure protection for everyone in healthcare facilities, thereby reducing the spread of SARS-CoV-2 within healthcare facilities. However, with the end of the “public health emergency”, many medical centers in the United States now no longer require the wearing of masks for all staff, returning (as was the case before the epidemic) to requiring the wearing of masks only in certain circumstances (such as when medical staff treat potentially infectious respiratory infections).
It is reasonable that masks should no longer be required outside of health care facilities. The immunity gained from vaccination and infection with the virus, combined with the availability of rapid diagnostic methods and effective treatment options, has significantly reduced the morbidity and mortality associated with SARS-CoV-2. Most SARS-CoV-2 infections are no more troublesome than the flu and other respiratory viruses that most of us have tolerated for so long that we don’t feel compelled to wear masks.
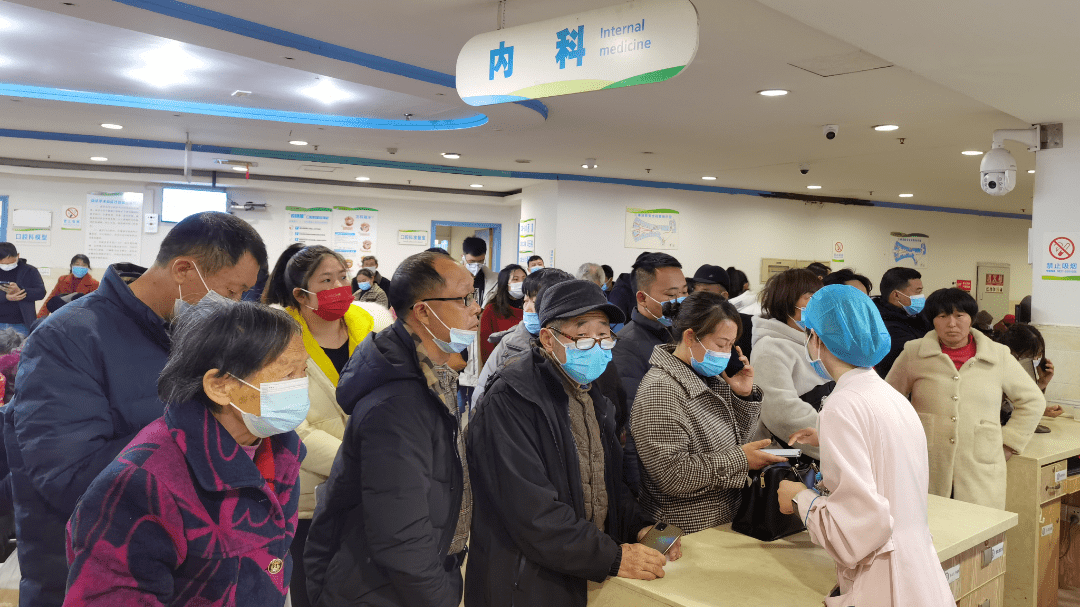
But the analogy doesn’t quite apply to healthcare, for two reasons. First, hospitalized patients are different from the non-hospitalized population. As the name suggests, hospitals gather the most vulnerable people in the whole society, and they are in a very vulnerable state (i.e. emergency). Vaccines and treatments against SARS-CoV-2 have reduced morbidity and mortality associated with SARS-CoV-2 infection in most populations, but some populations remain at higher risk of severe illness and death, including the elderly, immunocompromised populations, and people with serious comorbidivities, such as chronic lung or heart disease. These population members make up a large proportion of hospitalized patients at any given time, and many of them also make frequent outpatient visits.
Second, nosocomial infections caused by respiratory viruses other than SARS-CoV-2 are common but underappreciated, as are the adverse effects these viruses can have on the health of vulnerable patients. Influenza, respiratory syncytial virus (RSV), human metapneumovirus, parinfluenza virus and other respiratory viruses have a surprisingly high frequency of nosocomial transmission and case clusters. At least one in five cases of hospital-acquired pneumonia may be caused by a virus, rather than by bacteria.
In addition, diseases associated with respiratory viruses are not limited to pneumonia. The virus can also lead to the aggravation of the underlying diseases of patients, which can cause great harm. Acute respiratory viral infection is a recognized cause of obstructive pulmonary disease, exacerbation of heart failure, arrhythmia, ischemic events, neurological events and death. Flu alone is associated with up to 50,000 deaths in the United States each year. Measures aimed at mitigating influenza-related harms, such as vaccination, can reduce the incidence of ischemic events, arrhythmias, heart failure exacerbations, and death in high-risk patients.
From these perspectives, wearing masks in health care facilities still makes sense. Masks reduce the spread of respiratory viruses from both confirmed and unconfirmed infected people. SARS-CoV-2, influenza viruses, RSV, and other respiratory viruses can cause mild and asymptomatic infections, so workers and visitors may not be aware that they are infected, but asymptomatic and pre-symptomatic people are still contagious and can spread the infection to patients.
Generally speaking, “presenteeism” (coming to work despite feeling ill) remains widespread, despite repeated requests from health system leaders for symptomatic workers to stay home. Even at the height of the outbreak, some health systems reported that 50% of staff diagnosed with SARS-CoV-2 came to work with symptoms. Studies before and during the outbreak suggest that wearing masks by health care workers can reduce hospital-acquired respiratory viral infections by about 60%
Post time: Jul-22-2023