Can tissue samples be collected from healthy people to advance medical progress?
How to strike a balance between scientific objectives, potential risks, and the interests of participants?
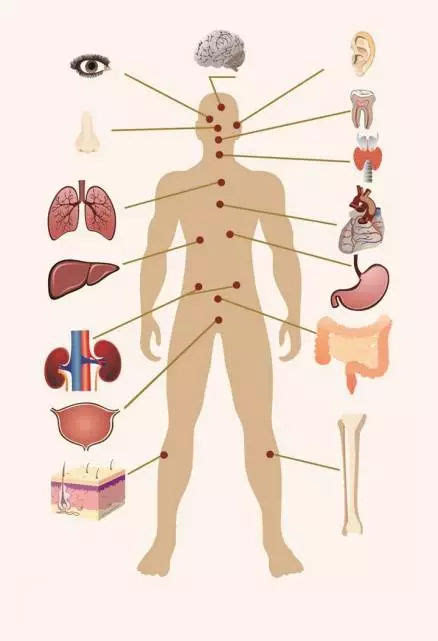
In response to the call for precision medicine, some clinical and basic scientists have shifted from assessing which interventions are safe and effective for most patients to a more refined approach aimed at finding the right therapy for the right patient at the right time. Scientific advances, initially embodied in the field of oncology, have shown that clinical classes can be subdivided into molecular intrinsic phenotypes, with different trajectories and different therapeutic responses. In order to describe the characteristics of different cell types and pathological entities, scientists have established tissue maps.
To promote Kidney disease research, the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) held a workshop in 2017 Attendees included basic scientists, nephrologists, federal regulators, Institutional Review Board (IRB) chairs, and perhaps most importantly, patients. Seminar members discussed the scientific value and ethical acceptability of kidney biopsies in people who do not need them in clinical care because they carry a small but clear risk of death. Contemporary “omics” techniques (molecular research methods such as genomics, epigenomics, proteomics, and metabolomics) can be applied to tissue analysis to elucidate previously unknown disease pathways and identify potential targets for drug intervention. Participants agreed that kidney biopsies are acceptable solely for research purposes, provided they are limited to adults who give consent, understand the risks and have no personal interest, that the information obtained is used to improve patient well-being and scientific knowledge, and that the review body, the IRB, approves the study.
Following this recommendation, in September 2017, the NIDDK-funded Kidney Precision Medicine Project (KPMP) established six recruitment sites to collect tissue from patients with kidney disease who had no indication of clinical biopsy. A total of 156 biopsies were performed during the first five years of the study, including 42 in patients with acute kidney injury and 114 in patients with chronic kidney disease. No deaths occurred, and complications including symptomatic and asymptomatic bleeding were consistent with those described in the literature and study consent forms.
Omics research raises a key scientific question: How does tissue collected from patients with disease compare to “normal” and “reference” tissue? This scientific question in turn raises an important ethical question: Is it ethically acceptable to take tissue samples from healthy volunteers so that they can be compared with patient tissue samples? This question is not limited to kidney disease research. Collecting healthy reference tissues has the potential to advance research into a range of diseases. But the risks associated with collecting tissue from different organs vary depending on tissue accessibility.
Post time: Nov-18-2023